Enterocytes
Section 6.1
(Published June 3rd, 2024)
| 🇨🇦 | 🕆 | 🇨🇦 | 🕆 | 🇨🇦 | 🕆 | L🇨🇦 |
6.1.0 Enterocytes, General Description and Scope
Enterocytes, are the nutrient absorbing cells which line the epithelium (inner surface area) of the intestinal tract. These are general-purpose absorptive-cells, which populate the epithelium of both the small and large intestines. The absorption process begins, once the stomach acids and digestive-tract enzymes have simplified food-stuffs in preparation. Most of our nutrients are absorbed within the small intestine, and there are higher populations of enterocytes within the smaller-diameter intestine versus the larger one.
Occasionally, you may run across the term “colonocyte” for this same type of cell. A colonocyte is the name reserved for nutrient-absorptive cells restricted to the colon of the large intestine. To date, I don’t believe there’s a physical difference between an enterocyte and a colonocyte. As a result, I will refrain from using the term colonocyte; and refer to all human nutrient-absorptive cells as enterocytes, regardless of their location.
I believe it’s commonly understood that all enterocytes are general-purpose in nature. Meaning, each cell has the capability of absorbing either fat, carbohydrates, proteins, minerals, water, or vitamins. It seems enterocytes by themselves, cannot selectively absorb one form of nutrient over another. Nonetheless, a natural selection process occurs due to an enterocyte's location.
Certain foods degrade faster than others, so foods capable of degrading quickly – are likely absorbed in the duodenum, which is located immediately after the stomach. The foods which degrade slower and are less nutrient dense, would likely be absorbed in the jejunum and ileum.
Certain enzymes, co-enzymes and pH levels; comprise the methodology and so-called "tools" of the digestive system. Generally, this is what controls the rate of chemical-breakdown and provides for an effective and efficient rate of nutrient-absorption. I assume that the varying density of enterocytes from one end of the intestine to the other, reflect its overall and ideal rate of nutrient absorption. However, due to disease and wear and tear, enterocyte densities can change over time.
Mature enterocytes survive for just four to five days before they either die or become sloughed off, and get pulled through the digestive tract. Due to this occurrence, once dead enterocytes become decomposed - they are free game for live enterocytes further downstream, to gobble them up. Particularly since the greater portion of a cell’s membrane is comprised of fatty acids, and free fatty-acids are easily absorbed by enterocytes
Further, it has been considered that one of the reasons why enterocytes become sloughed off, is due to them being chock full of nutrients. From this stance, it’s assumed that while the enterocyte has done its job of absorbing as many nutrients (such as amino-acids) as it can - the body may not be prepared to accommodate further nutrients at that particular time. If this is the case, then the enterocyte makes the ultimate sacrifice (apoptosis) in hopes that its cell and previously-ingested nutrients can be used later, and further down the digestive tract.
I believe that the primary reason why enterocytes have such a short lifespan, is to ward off pathogens which may infiltrate the digestive tract. As far as cells go, enterocytes are comparatively mobile, and migrate along their underlying basement-membrane. Even while a pathogen infects a single enterocyte, the chance of it spreading from one cell to the next is rather slim. The short life-cycle of enterocytes, certainly restricts the number of pathogens capable of hindering a group of them at once.
It has been determined, that even without enterocytes themselves, a certain percentage of ingested water and small molecules can be absorbed directly through the walls of the stomach. I understand that ethanol (from alcohol), caffeine, drugs, and amino acids, can be absorbed through the stomach lining and directly into the bloodstream. Due to its convenient and quick nutrient-absorption capability, drug companies often target the stomach itself.
Most of our nutrients are absorbed within the small intestine, and more specifically - the duodenum and jejunum. Digestive bile and digestive salts which can be later recovered, is done so within the ileum, which is the distal and third section of the small intestine.
What is often overlooked with regards to the digestive process, is the fact that the large intestine can absorb nutrients as well. By the time food remnants reach our large intestine, most of their nutrients have already been ingested. Interestingly, this is the location where the gut’s microbiome and its bacterial colonies rise to the occasion.
Bacteria and notably the good bacteria (probiotics), feed upon digested remnants which had been previously discarded. Basically, bacteria have the ability to transform what was once expelled biological-waste, and turn it into something that’s beneficial for the body. An example of this, is the water-soluble vitamin B12.
Appropriate strains of gut bacteria, manufacture B12 from digestive-waste-products and merely discard it into the intestinal lumen. Once this occurs, colonic enterocytes absorb vitamin-B12 if they wish to do so. In effect, this should negate the “fact” that we all need to ingest B12 from animal products in order to remain healthy. Unfortunately, the quantity of beneficial bacteria within our gut (probiotics) is minimal, and we likely don’t have sufficient bacterial-colonies capable of sustaining a healthy reservoir of vitamin B12.
Due to the following reasons, proliferation of our gut’s bacteria is continually being restricted.
- Chlorine in the local drinking-water kills both good and bad bacteria.
- An acidic-diet leads to an unhealthy relationship of good bacteria versus the bad. As a consequence, an unhealthy microbiome results.
- Medications and use of antibiotics kill off good bacteria.
- Removal of one’s appendix, leaves minimal undisturbed surface areas (within the intestines) for bacterial colonies.
For all the reasons I’ve just mentioned, I surmise that our large intestine likely absorbs only about five to ten-percent, of the amount of nutrients for which it was originally intended.
Further, as water is released from the small intestine into the larger one, a water gradient naturally occurs throughout the stool of the large intestine. I believe that the large intestine not only absorbs water, but also serves as a means of water secretion. In essence, the large intestine regulates water distribution throughout its entire length. Hence, it should be able to control the wet/dry transition which is central to the bowel.
If bacterial colonies within the gut are generally separated by being either aerobic (require oxygen) or anaerobic (can live without oxygen) - then the oxygen-carrying water serves to regulate proliferation of certain bacterial-strains. I gather that most colonies of aerobic bacteria are stored within the cecum and appendix, whereas colonies of anaerobic bacteria are stored distally in the large intestine. Notably, most bacteria of discharged fecal matter are anaerobic.
If aerobic-bacteria release specific types of vitamins as waste products, and anaerobic-bacteria release opposing types of vitamins as waste products…. then the large-intestine is capable of regulating its absorption of nutrients, merely by regulating fecal-water content.
As a result, our large-intestine has the ability to control its intake of certain nutrients, regardless of the fact that these nutrients were never ingested through our mouth.
6.1.1 Specific Processes of Enterocytes
The following drawing shows enterocyte cells lining the intestinal epithelium, as well as certain methodologies in which they ingest our body's nutrients.
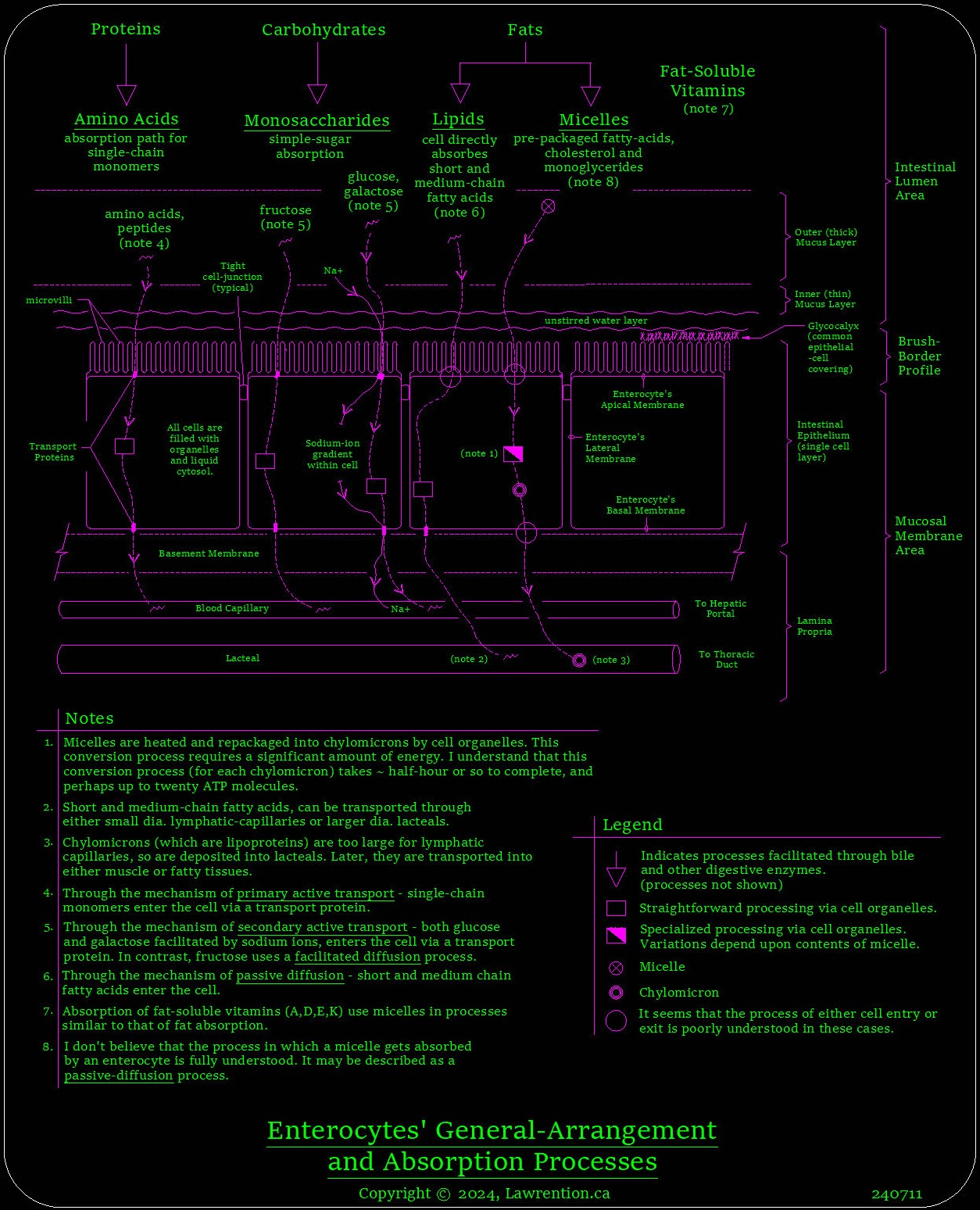
At the top of the drawing, we have proteins, carbohydrates, and fats entering the lumen of the intestine. The GI-tract uses both mechanical means and chemically-based digestive-enzymes, in order to break down common food-stuffs into their simpler constituents. These simple constituents can then be directly absorbed by enterocytes. Other than water itself; proteins, carbohydrates and fats, comprise the bulk of ingested nutrients. These three basic groups of nutrients, are perhaps the simplest to explain as to how they get ingested.
At the far left of the drawing, it shows how amino acids and peptides enter an enterocyte. They do so through a transport protein which spans the complete thickness of the cell’s membrane (transmembrane protein). These simple constituents are basically string-like structures which can be absorbed easily via transport proteins. They are absorbed through a process requiring energy, and this process is referred to as primary active transport. The term primary verses secondary becomes rather obvious, as we will see shortly.
“Active” infers that this process requires a supply of energy in order to move past an electrochemical gradient, and for the molecule in question to pass through a cell’s membrane. In this case, the energy required for either amino-acid or peptide absorption through primary active transport, comes from molecular ATP (adenosine triphosphate) within the cell.
Transport proteins are uniquely structured, and only allow certain (molecular) structures to pass through. Some transport proteins accept just one type of molecule, whereas others provide a means for a few different types to pass on through.
I suspect that under ideal circumstances, a molecular chain-like structure such as amino-acids, can both enter and exit an enterocyte at virtually the same rate. After all, enterocytes have been developed over numerous generations, and first existed millions of years ago. For myself, this raises certain questions, like: how are absorption rates regulated? Are enterocytes allowed to merely absorb whatever is available at the time? And when one type of nutrient is preferred over another, by one’s body (systemically) - how is this regulation coordinated through the digestive-system? Can an enterocyte absorb two different types of nutrients at once?
Setting all of these questions aside for the time being, let’s return to the drawing at hand, and review the ingestion process for simple sugars (monosaccharides). Our current example, refers to the second cell from the left. Here, both glucose and galactose are absorbed by using a process referred to as secondary active transport.
For absorption of either a glucose or galactose molecule to occur, a sodium ion has to be absorbed at the same time. This is why the process is named secondary active transport, as it needs a secondary molecular-structure to be absorbed alongside the primary one’s path. The idea of having two different types of molecules passing through a single transport protein at the same time, distinguishes secondary-active transport from primary-active transport.
For fructose absorption, it is deemed to be a facilitated diffusion process. Unfortunately, the facilitated part of this process is not fully understood. Here, the rate of uptake relies primarily upon the fructose-concentration gradient across the cell’s membrane. However, there are also factors yet to be determined, which is the facilitated part of process. This as of yet, unknown facilitated part - is what prevents this process from being totally linear in nature.
Inside enterocyte cells are its organelles and cytosol. Organelles to cells, are analogous to the multiple organs within our body. Each cell has a number of organelles, and each organelle has its own set of unique functions. The clear aqueous fluid in which these organelles are suspended in, is referred to as the cell’s cytosol.
On our prior drawing, there are square boxes which represent straightforward processing methodology by the cell’s organelles. As an explanation, this means that the processing for certain molecules (nutrients) entering the cell, can be done relatively efficiently and easily. Here, minimal modifications are required to both process and transport the molecule in question. In contrast, when it comes to the absorption of fats by using intermediary micelles - it takes much more processing effort from a cell’s organelles, in order to modify the fat-globule and later deposit it into a local lacteal.
Through a passive diffusion process, enterocytes can absorb both short and medium-chain fatty acids. As far as the cell is concerned, these can be processed in a straightforward manner and later deposited into a nearby lacteal.
In order to isolate fat globules from the aqueous fluid in the small-intestine’s lumen, bile is released into the gut. This bile emulsifies lipids and facilitates the creation of micelles “on the fly”, so to speak. Through this natural (phospholipid) process, fats gather together in clumps – and form smooth circular-shaped micelles. Since semi-digested fats come in various forms and often include fat-soluble vitamins as well… a micelle's contents are a mixture of various molecular species.
Micelles are absorbed by enterocytes through a passive-diffusion process. This process is not well understood, although I believe it doesn’t require a transport protein. It seems that it’s more of a phospholipid exchange and/or manipulation process, as it passes through the membrane. There’s no need for a transport/transmembrane protein whatsoever.
Once a micelle enters an enterocyte, it needs to be processed and converted into a chylomicron. From what I understand, the greater portion of these chylomicrons are made up of triglycerides. Specific proteins (apolipoproteins) bind with chylomicrons during the manufacturing process within the cell.
Through a minimal understanding of chylomicrons, I believe that its contents are both categorized, and characterized, by both its physical size, and the type of apolipoproteins exposed on its exterior. Once a chylomicron makes its way into the bloodstream, it can be appropriately flagged and guided towards the proper tissue areas and applicable cells. Chylomicron remnants, are later processed by the liver.
Enterocyte Weight-Loss Mechanism
6.1.2
The greater portion of a chylomicron's mass is due to its triglycerides. Triglycerides are an excellent source of energy for the body, so this is why it likes to store them (or their simpler constituents) within cells. Triglycerides are abundant within one’s bloodstream, and an overabundance increases the risk of heart-disease.
As I alluded to previously, it takes a tremendous amount of energy to create chylomicrons from micelles. I surmise that there’s also a certain amount of ATP required for an enterocyte’s maintenance, and at certain times - a greater amount is required to process incoming nutrients. Especially if an enterocyte is processing micelles, as I believe an internal heating-process takes place which requires gobs of energy. As far as processing micelles go (via organelles), due to both the energy-aspect and the potential number of molecular variations which might occur in order to form chylomicrons - I refer to this method as being specialized.
In this specialized-processing scenario, since there’s so much energy required, enterocytes eventually extinguish their ATP reserves, and cease to function. As cell ATP reserves fall, these enterocytes are no longer capable of absorbing fat. Other nutrients, perhaps - but not fat absorption via the micelle process.... it's not possible.
Once chylomicron production halts, blood-triglycerides begin to fall. Once blood-triglycerides fall, its impossible to gain more weight. In fact, the body begins to use fat-reserves for energy instead of glucose, and the weight-loss process begins.
Now, I know that this concept works, as it’s worked for me. In our modern upside-down world, it’s the sugar and carbs which are often the culprits, not the proteins and fats! The downside here, is that once carbohydrate intake resumes again - shortly thereafter, and once enterocytes restore ATP reserves... they are primed for fat absorption.
Given the choice, our cells prefer simple sugars over fats for energy. I can’t say for sure why our body functions this way, I can only speculate that it was done as a survival mechanism. Sugars are absorbed quickly and used quickly, whereas most of our fats (at least those absorbed through micelles) - are absorbed comparatively slower, and utilized sparingly.
Personal Experience
As for myself, my blood-triglycerides were once so high -I was likely going to have heart problems before I was forty years of age. I didn’t have any symptoms, as the problem was only discovered when the doctor suggested I might want to follow up with a specific triglyceride/lipid profile blood-test.
I wasn’t extremely overweight at the time (twenty pounds likely), but for whatever reason… my blood-triglycerides were through the roof. From what I’ve since discovered - it seems that some people can have consistently high triglycerides, but do not necessarily gain much weight, if any.
Prior to starting what I would call a protein/fat diet, I had tried for perhaps a couple of years to no avail, as I attempted to improve my blood’s triglyceride/lipid profile. I had restricted my intake of eggs, meat, dairy, etc., but all of it had minimal impact. I certainly had my fill of melba toast which was dry as dust!
Finally, I purchased a book called Protein Power, and followed its instructions as best I could. It offered some hope, as there were many people out there which had the same problem.
As I began the diet, I started out with a big breakfast of eggs and bacon – no juice or toast, it was either water or coffee. I remember telling my wife, that it was either going to cure me or kill me. Previously, I had restricted my diet to no bacon whatsoever, and about three or four eggs a week; so this was a refreshing change. For lunch, it was often beans and tuna, and a hand-full of almonds. Lots of cottage cheese, meat without carbs, and non-battered fish, was the flavour of the day. If I ate a hamburger, I would eat it without the bun. Any nuts or seeds which tasted good was a bonus.
After about the first week, I began to add some greens and salads. I believe that the idea of the diet’s first week or so… was to make one’s body sensitive to carbohydrates again. Due to insulin resistance, the body tends to store fat and causes ravaging hunger.
When I started this protein diet, I found that for the most part, I was no longer hungry, and had no loss of energy. In fact, at times - it seemed like I had even more energy than prior. Whenever I got hungry, food cravings were typically quenched by eating more protein.
As the weeks went by, I gradually began to add more fruits and vegetables. After about a month and a half, I had another blood test. Surprisingly, my lipid profile was great, and overall triglycerides were about a tenth of where they were had been originally. My triglyceride levels were now at about half the level which the doctor considered to be normal! At the time, the doctor’s assistant said that I was “cured” and had triglyceride levels like that of a runner. Oh, and by the way - I lost about fifteen pounds in one month’s time.
Over the years, whenever my health seems to go off the rails, I return to this diet. It seems to work great for the short term, but after a while one tends to get sick of all the proteins and fats. As well, eating lots of cheese with little fiber, can be a real issue.
It seems that a lot of our health issues stem from the fact that we certainly don't eat or exercise like our ancestors did. I gather that minimally, our ancestral lines were biased towards either farming, hunting, or fishing, and their respective environments. If you look on maps which reveal population densities, it's easy to see that most people (two-thirds perhaps?) tend to live near a body of water. This likely held true for generations of the past as well.
Full Disclosure Statement: Please be well aware that I am not a health professional. The information herein is based upon personal life-experiences, research, and knowledge of certain topics which the Lord has graciously guided me through.
Take-note that certain unique information herein, of which there’s a substantial part; has yet to be evaluated by the health-care industry. So, as always, heed the advice of your physician and ask for their advice, before varying either diet or lifestyle.
We understand that the human body is comprised of trillions of cells and is quite complex. Hence, a little common sense reminds us of the fact that we need a certain length of time to change the course of our health. This includes of course, our daily habits.
Lawrention
If you wish to understand certain points on nutrient absorption which I’ve failed to mention, there’s a great summary from: Eric J. Basile, Marjorie V. Launico, and Amy J. Sheer; entitled: "Physiology, Nutrient Absorption", dated October 28, 2023.
(Back to H&L Contents)
Rev. 250516